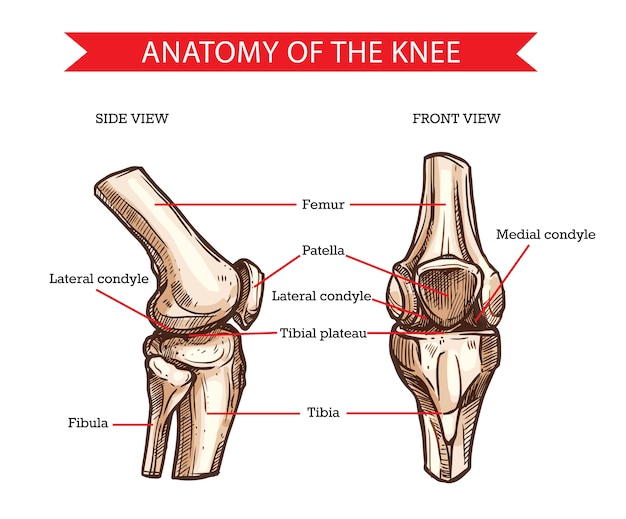
The knee joint is made up of the femur (thigh bone), tibia (lower leg bone), and patella (kneecap). These three bones are held together and supported by the soft tissues (muscles, tendons, ligaments) that surround the knee.
Additionally, the surfaces of the bones are protected and cushioned by cartilage and menisci which also help to absorb shock within the knee joint. It is very common to experience knee pain and this pain can occur due to an injury or dysfunction in any of the structures that make up the knee.
The knee is involved in many different movements for a variety of activities, occupations, and sports and can often be put into positions that increase stress on the structures or be subject to forces that disrupt its function and can lead to an array of injuries. The following are some injuries that can occur in and around the knee.
Knee Injuries
Iliotibial Band Syndrome (ITBS)
The iliotibial band, also known and the IT band, is a strip of fascia that runs from the pelvis to the outside region of the knee. It can result in pain or discomfort on the outside of the thigh down to the outside part of the knee.
There are also a few muscles that attach to the IT band which can influence how it moves and cause pain as well. Knee pain can result when the IT band rubs over the part of the femur which makes up the knee.
As the knee is bent and straightened the IT band will move back and forth which can create friction and can cause damage in the IT band which can result in inflammation and pain. If the muscles that attach to the IT band are tight, they can pull on the IT band causing it to tighten which then leads to compression on the structures underneath and this can also result in knee pain.
This syndrome is commonly seen in runners, cyclists, and hikers and is thought to be due to muscle imbalances, decreased mobility, and non-optimal training habits ( too much too fast, an incomplete training plan. Your therapist can assess these imbalances and put you on the road to happy and healthy activity!
ITBS can be classified into acute if the onset of pain and discomfort has occurred for less than 6 weeks and in this stage, the IT band may be inflamed and actively trying to heal. When the injury lasts beyond 6 weeks and up to 12 weeks it can be considered sub-acute and if it has been occurring for longer than 12 weeks it can be considered chronic.
Patellar Tendinopathy
The patella, also known as the kneecap, is attached to the quadriceps muscles at the top and to the tibia (lower leg bone) at the bottom by a patellar tendon. This tendon allows the forces from the quadricep muscles to be used to straighten the knee and control the knee while it bends.
This tendon can be damaged and result in pain at the front of the knee. Typically, this injury occurs from overuse due to repetitive activities and loading.
Activities with repetitive loading such as cycling, sports involving jumping and landing like cross-fit, basketball, volleyball, or athletics or cutting activities like soccer, field hockey, and rugby, and even downhill running/hiking have big loads through the quadriceps muscles and the patella tendon.
The stress of these activities causes micro-tears and trauma in the tissue, which is normal, and the body will then respond by adapting to get stronger in order to better tolerate these types of activities in the future. In the case of patellar tendinopathy, the loading is occurring at a pace that is too quick for the tendon and muscles to recover and the micro-tears will then turn into overuse injuries.
This injury is typically classified based on how the pain presents.
- When the pain occurs after activities it is a Grade I classification;
- Grade II is when the pain occurs at the beginning of activities but is relieved once the tissues have warmed up;
- In a Grade III the pain is constant and occurs at rest and during activities; and
- A Grade IV is a complete rupture of the tendon.
Patellofemoral Pain Syndrome
During knee movements, the patella (kneecap) will move up and down a groove in the femur and there is cartilage on the surfaces which allows the movement to be smooth and have minimal friction.
Patellofemoral pain can occur at the front of the knee and around the sides of the patella and can come from the bone, the cartilage, the joint capsule, or the fat pat under the patella.
To function optimally, the patella required adequate passive stabilization from the soft tissues that surround it and active stabilization from the muscles surrounding the hip and knee. Typically, this injury occurs from overuse and increased loading in the knee joint.
For example, a rapid increase in running distances or the intensity of the runs can be a mechanism of injury. Additionally, if there are dysfunctional movements within the hip, ankle, and foot it can increase the loading that occurs at the knee and contribute to the development of patellofemoral pain.
When there is suboptimal alignment and biomechanics within the knee joint it can alter the forces within the knee and overload the tissues and cause irritation and pain. The patellofemoral pain can be started by trauma to the patella which alters its stability and movement within the joint.
Additionally, it can be due to non-contact reasons related to a variety of different variables. These variables can be related to overloading, repetitive loading, muscle weakness, muscle imbalances, or biomechanical abnormalities. Alternatively, the pain can be due to dysfunction in other areas which results in pain within the knee.
Patellofemoral pain syndrome can be classified as acute if the onset of pain and discomfort has occurred for less than 6 weeks. When the injury has lasted beyond 6 weeks it can be considered sub-acute and if it has extended beyond 12 weeks it can be classified as chronic.
It is common for those involved in activities such as cycling and running, sports that involve jumping, running, and cutting (for example volleyball, soccer, basketball, field hockey, ice hockey, rugby), or those that involve heavy loads and plyometrics (boot camps, cross fit, weight lifting) to experience PFPS.
Patella Dislocation
During knee movements, the patella (kneecap) will move up and down a groove in the femur. In some instances, the patella can be dislocated which means the patella moves out of the groove on the femur and this typically occurs towards the outside of the knee.
This injury can occur due to direct impacts to the patella which forces it into dislocation or through non-contact mechanisms where the knee is placed in a non-optimal position and the muscles and soft tissue surrounding the patella are unable to maintain their stability.
Knee Ligament Injuries
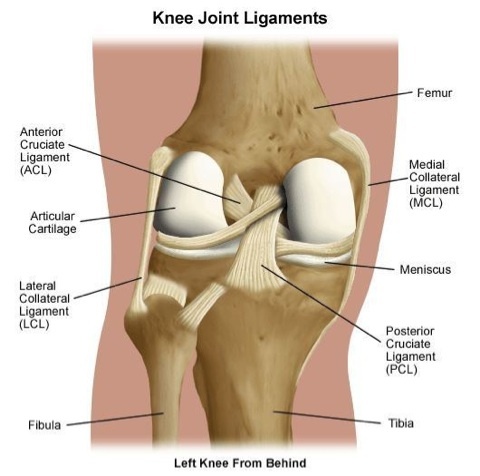
ACL: The anterior cruciate ligament, also known as the ACL, runs in the inside of the knee joint between the femur and the tibia. Its role is to resist the movement of the tibia forwards or excessive rotation within the knee joint.
This is the most injured knee ligament.
This ligament can be injured due to contact mechanisms or through non-contact mechanisms such as changing direction, pivoting, or a poor landing after a jump. This is a common injury in running and cutting sports ( for example soccer, rugby, basketball, field hockey, football) as well as skiing and snowboarding.
PCL: The posterior cruciate ligament, also known and the PCL, runs in the inside of the knee joint between the femur and the tibia and creates an “X” with the ACL. Its role is to resist movement of the tibia backward or excessive rotation within the knee.
This ligament is not commonly injured, as compared to the ACL.
The mechanism of injury is typically an impact to the tibia or knee which results in backward movement of the bone. This could occur by falling hard onto the shin or hitting the knee on the dashboard during a car accident.
MCL: The medial collateral ligament, also known as the MCL, runs on the inside part of the leg from the femur to the tibia and crosses over the knee joint line. Its main role is to resist inward forces on the knee, also known as valgus forces, and provide stability to the knee joint.
This is a common injury in sports such as soccer, football, and rugby where the knee can be easily impacted on the outside and be forced inwards while the foot is planted. Alternatively, it can be injured while completing pivoting maneuvers or while catching an edge in skiing.
These mechanisms will cause the knee to move inward at the same time as applying rotation forces to the knee which causes stretching and stresses within the medial collateral ligament. Typically, this ligament is injured alongside other structures in the knee.
LCL: The lateral collateral ligament, also known and the LCL, runs on the outside part of the leg from the femur to the tibia and crosses over the knee joint line. Its main role is to resist outward forces on the knee, also known as varus forces, and provide stability to the knee joint.
This ligament is injured less often as compared to the MCL.
When an injury occurs in this ligament it typically is in sports such as soccer, basketball, tennis, and gymnastics which can create stresses and hyperextension at the knee and cause damage to the lateral collateral ligament. It can also be caused by an impact on the inside of the knee causing it to move outwards while the foot is planted.
Ligament injuries around the knee can be classified into grades.
- Grade I occurs when the damage to the ligament is minor and there are only microscopic tears which results in some minor tenderness and pain but does not result in joint instability;
- Grade II is considered a partial rupture where more of the fibers have been torn and this can result in moderate to major tenderness and pain and may cause mild instability at the joint;
- Grade III is a complete rupture of the ligament, which means all of the fibers have been torn and this will lead to an unstable joint.
Knee Meniscus
There are two menisci in the knee joint. They sit between the femur (thigh bone) and the tibia (lower leg bone) on the left and right sides of the knee joint. The meniscus is made of cartilage and its role is to provide stability, cushioning, and shock absorption within the knee.
Injury to the meniscus is the second most common knee injury.
The meniscus can be torn or injured by traumatic or degenerative mechanisms. As people age the meniscus will degenerate as the cartilage changes with age or other processes such as osteoarthritis.
This degeneration may result in small or larger tears within the meniscus which can result in pain or discomfort in the knee joint. The menisci can also be injured through traumatic mechanisms such as rotation with straightening or bending the knee which can cause compression and tearing within the meniscus, which is more common in younger populations.
These meniscus injuries can be classified based on the variety of tears which can occur, but generally, the treatment remains similar despite the type of tear.
Knee Osteoarthritis
Osteoarthritis is another common cause of knee pain.
Osteoarthritis impacts all the structures that make up the joint and through repeated loading and inflammation the cartilage and structures around the joint will start to degrade and change.
Knee OA can be classified into primary OA where there is no clear cause or factors related to the degeneration or secondary OA where there are underlying factors such as hypermobility, diabetes, trauma, or sports-related injuries which have influenced the health of the knee joint.
As the knee joint degenerates with OA, there is often loss of joint space, growth of new bones known as osteophytes, changes in the bone density, and formation of cysts.
The stages of OA can be graded from 0-4 based on the stages of the changes that have occurred. Despite having an x-ray as a useful tool for diagnosing OA, Physiotherapists also have a variety of screening measures used to identify those with OA and rule out other serious red flags or conditions.
What to expect during your appointment for a Knee Injury Physiotherapy in North Vancouver?
Regardless of the cause of your knee pain and dysfunction, Cypress physiotherapy in North Vancouver is an excellent tool to help you manage and improve your function. During the appointment, we will provide an assessment that is individually tailored to your knee injury.
This will include gathering a detailed history from you and spending some time to identify mechanisms of injury or any underlying causes of your knee dysfunction. From there, we will perform a detailed assessment of your knee and will also look at your hip, ankle, and foot as dysfunction in these regions can often lead to pain and dysfunction within the knee.
Our Cypress physiotherapists in North Vancouver have extensive training that allows them to test a variety of structures around the knee and determine the cause of your knee pain and the structures involved. This process will help us to develop a rehabilitation plan tailored to your specific individual needs.
Depending on the type of knee injury you are experiencing, we may use a variety of physiotherapy treatment techniques. You can expect to receive adequate education on your knee injury, risk factors, prognosis, re-injury prevention, and the rehabilitation plan.
Our Cypress physiotherapists in North Vancouver will provide you with a therapeutic exercise plan to work on muscle strength, endurance, proprioception, motor control, and mobility around the knee and the joints above and below. Additionally, we may use other techniques such as IMS, manual therapy, return to sports training, and taping to supplement the rehabilitation.
In the instances where the injury requires surgery, we can provide prehab prior to the surgery and rehabilitation after the surgery in order to get you back to participating in your occupational and recreational activities. The recovery time will vary from injury to injury and will also depend on the grade or severity of the injury.
Generally, soft tissue healing takes 6-8 weeks and can extend beyond a year in cases such as an ACL rupture. By understanding the orthopedic and biomechanical underpinnings of how the body works, we can selectively employ the right techniques and create a sustainable and effective care plan to help you get your knee back to full, pain-free functioning and participating in the things and activities that you love.
Call or go online to book an appointment for your knee pain with Cypress Physiotherapy and Health in North Vancouver.